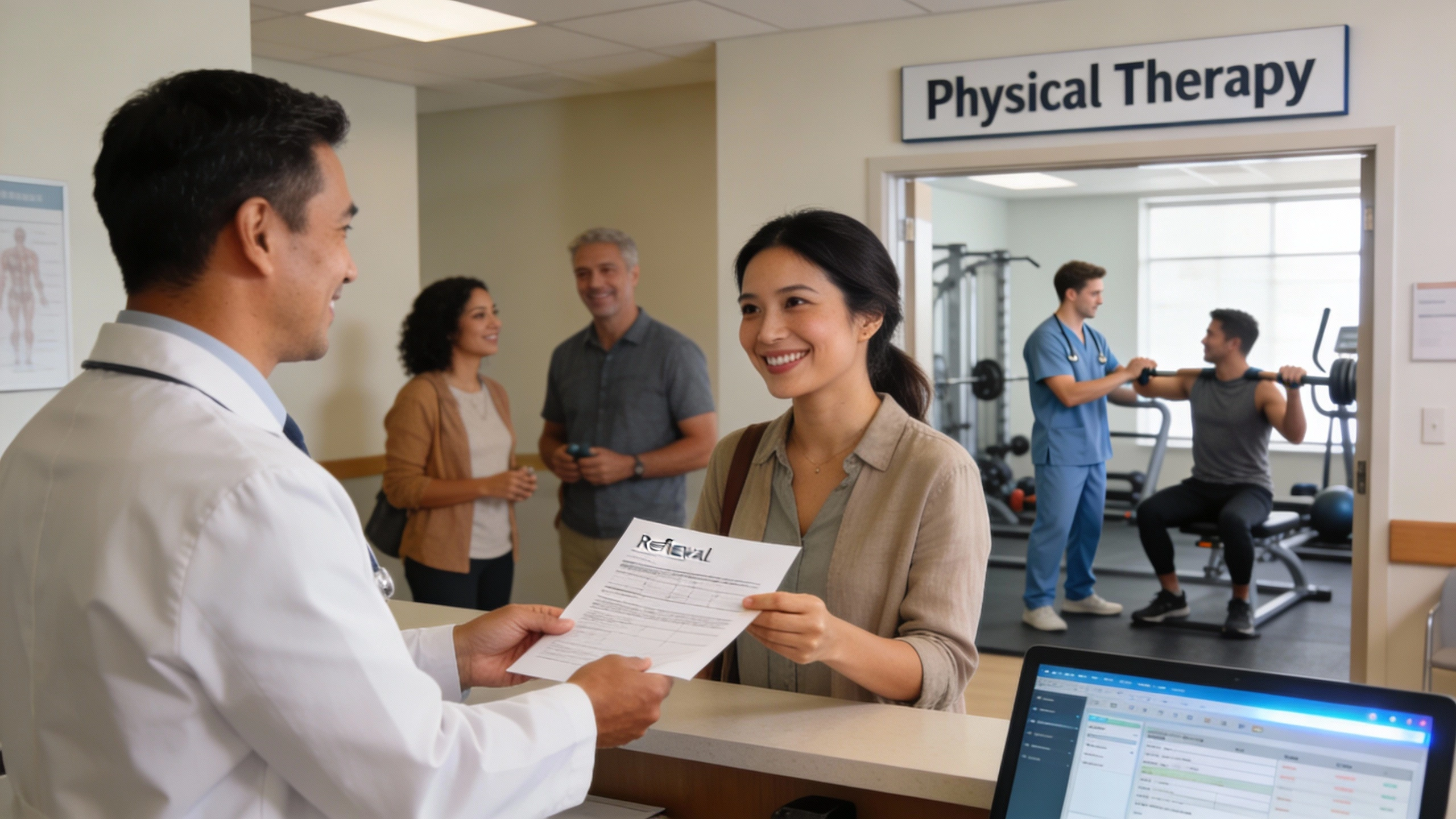
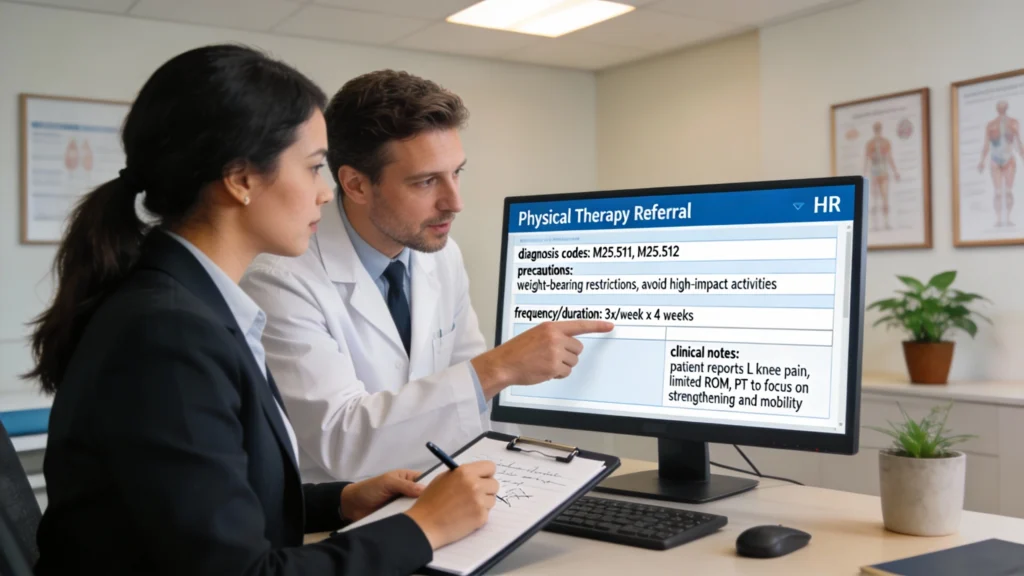
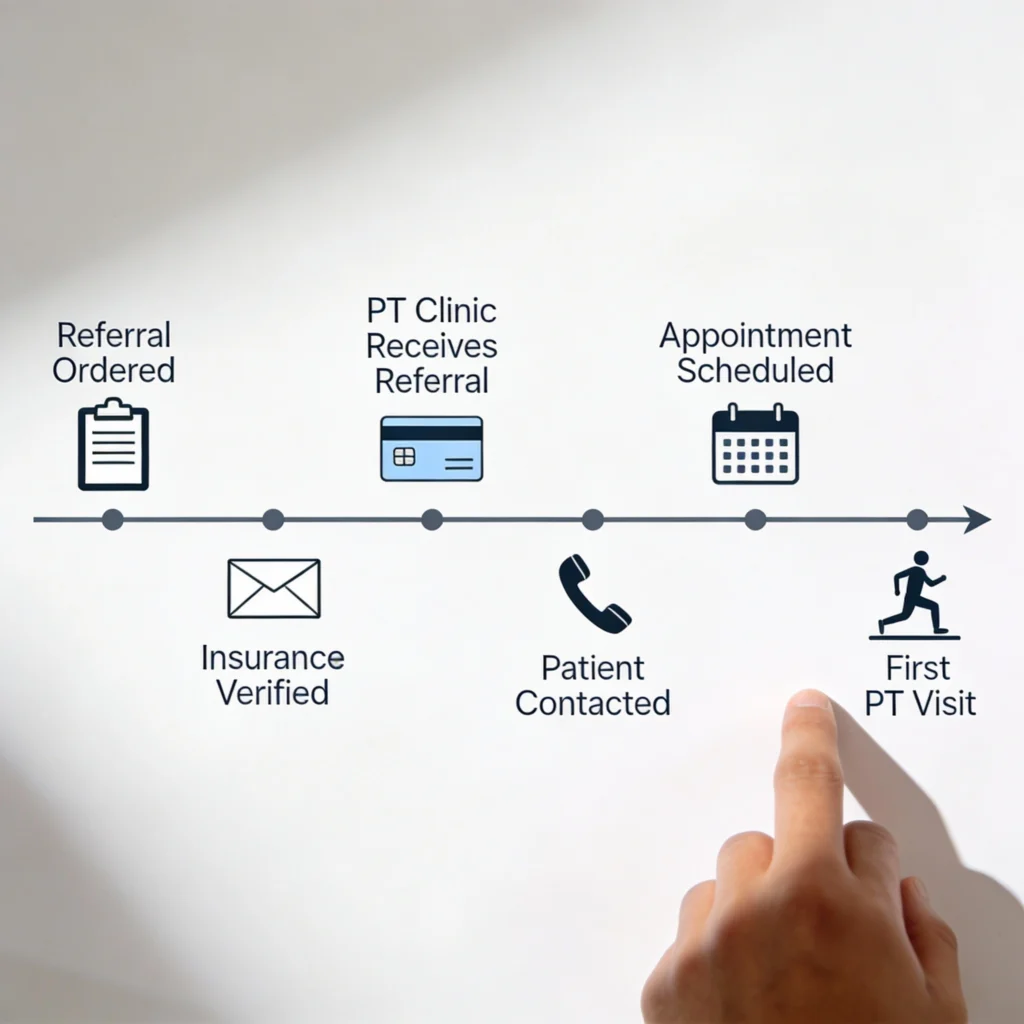
An ambulatory referral to physical therapy formally links an outpatient visit to a PT clinic, often through an electronic health record. Rather than a casual suggestion, it is a structured order that triggers scheduling, insurance checks, and documentation so the patient’s transition from medical evaluation to rehabilitation care is clear and timely.
Ambulatory referral to physical therapy describes sending a patient from an outpatient setting—such as primary care, orthopedics, or community clinics—to a PT provider. Unlike inpatient or acute care referrals, the patient is medically stable and living at home. The referral’s purpose is to address musculoskeletal, neurologic, or functional problems before they worsen or require hospitalization.
Ambulatory vs. Inpatient or Acute PT Referrals
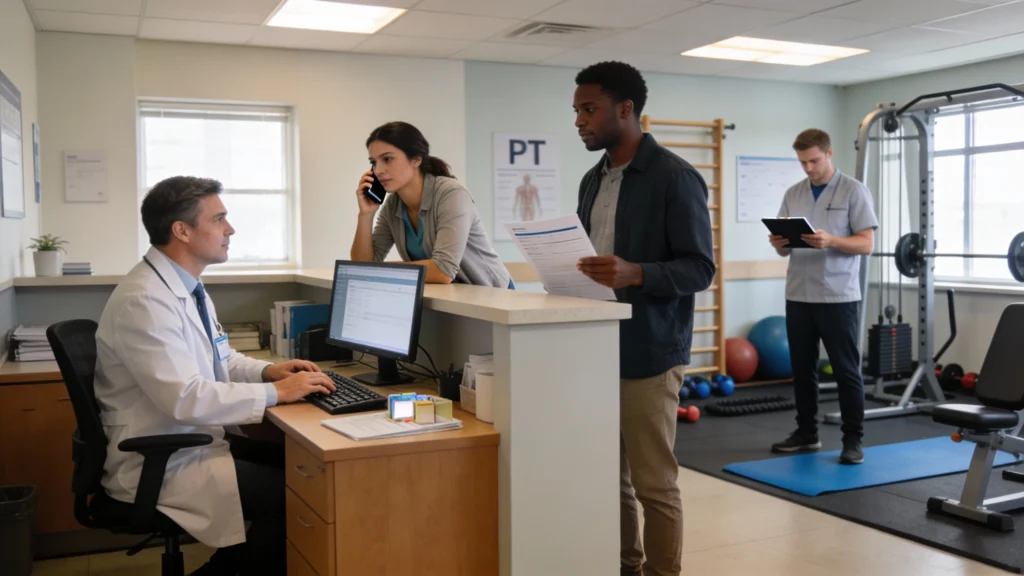
In inpatient or acute care, PT referrals occur inside the hospital, often within 24 hours of admission, and therapists treat patients at bedside. Ambulatory referral to physical therapy instead crosses organizational boundaries, frequently involving separate billing systems, prior authorizations, and patient self-transport. These referrals must account for clinic capacity, insurance networks, and patient preferences about location and schedule.
Typical Use Cases in Outpatient and Community Settings
Common ambulatory referral to physical therapy scenarios include post-surgical rehab after ACL reconstruction, chronic low back pain lasting over six weeks, or balance issues increasing fall risk. Community health centers may refer patients with diabetes for gait and foot-strengthening programs. Many systems also use standardized triggers, such as a Timed Up and Go score above 13.5 seconds, to automatically prompt PT referrals.